Background
In Ph+ALL patients, prophylactic/maintenance administrations of TKI are used after the protocol treatment. Unlike Chronic myelogenous leukemia (CML), after TKI stopped, there is no consensus about how often to monitor to detect molecular relapse. In the current study, from clinical data of 31 patients we tried to determine the optimal frequency of MRD monitor for better prognosis using a mathematical model.
Methods
Doubling time (DT) and Growth rate (GR) were retrospectively calculated by the increase of BCR-ABL from 99 kinetic data from 31 patients with Ph+ALL at molecular relapse. Measurement of amount BCR-ABL was performed by RQ-PCR. Mimicking CML, we defined BCR-ABL/ABL ratio of 0.1% as "MR3 (Major molecular response)" and undetectable levels of BCR-ABL transcript as "MR5 (Complete molecular response)". In order to investigate the relationship between tumor burden (BCR/ABL) at the time of MRD detection and prognosis, it was divided into 3 groups, BCR/ABL<0.1% (MR3), 0.1%<BCR/ABL<1% (MR2) and BCR/ABL>1% (MR1). This study was approved by the institutional review committee.
Results
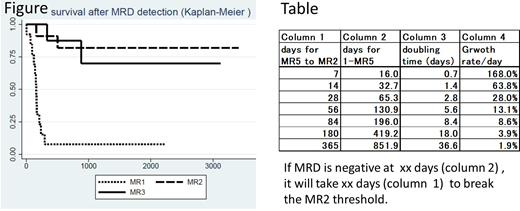
The doubling time was 1.3 days (GR 0.7%/day) to 95.4 days (70.8%/day) with a median of 12.3 days (5.8%). The rate of increase was compared by three groups of tumor burden. The DT among patients in MR1 was shorter than those in MR3 and MR2 (7.7 days vs 15.2 days in median, t-test p<0.01). There were no differences of DT in sex, age, treatments and BCR/ABL mutation. Most patient had multiple kinetic data and the smallest amount of BCR/ABL was used in each patient. Among 8 patients who showed MR3 (MR3pt) and 11 who showed MR2 (MR2pt), 14 are alive at this analysis, while among 10 patients who showed MR1 (MR1pt), only 1 patient is alive.(Log-rank test, p<0.1) (Figure) Median survival time is 882 days, 330 days and 16 days in MR3pt, Mr2pt and MR1pt, respectively. All patients died of progression of the disease. Finding molecular relapse before MR2 may related to better results.
Optimal interval of MRD detection
We set several hypotheses to determine the optimal frequency to detect early recurrence of leukemia. We estimated that patients with MR2 and MR5 have 1010 and 107 Ph+ cells in body, respectively. We defined "MR2" and "MR5" as "optimal intervention threshold" and "detection threshold". From our clinical data, we tentatively determined that doubling time of leukemia growth is distributed between 1 day (GR 100%/day) and 100days (0.7%). Also, we assumed that single cell has a relapse potency and the GR is constant during observation in each patient. The number of Ph+ cells in a MR5 patient who would potentially relapse might be distributed between 1 cell and 1 x 107 (MR5). "Success" was defined as if molecular relapse is detected between M5 and MR2 and "Failure" was defined as if detected more than MR2.
According to the daily clinical practice, the optimal examination interval is tentatively every 7 days, every 14 days, every 28 days, every 56 days, every 84 days, every 6 months, and every year. First, in order to calculate the growth rate that would be successful at 7-day intervals, the rate of 168%/day for 1 cell to increase 107 (MR5) in 7 days was calculated. This rate is faster than the maximum rate of 100%/day in this study, so an interval of 7 days is good for the initial period. Similarly, at 14-day intervals, 68%/day is calculated, and in this case, it requires 32 days to increase 107 (MR5) from 1 cell. As a result, after 32.7 days, 14-day intervals are acceptable. Similarly, the calculated results for 28 days, 56 days, 84 days, 6 months, and 1 year are shown in the Table. MRD can be found before M3 (success) with 28-day intervals after 65 days, 56-day intervals after 131 days, 84-day intervals after 196 days, 6-month intervals after 419 days and 1-year intervals after 852 days.
Conclusion
Taken together, soon after stop of TKI, more frequent monitoring of MRD than in "treatment free remission" in CML is needed. The interval can be prolonged with the passage of time. In several patients, hematopoietic stem cell transplantation (HSCT) was possible due to early intervention by changing TKI and chemotherapy. After HSCT, TKI combined with rapid reduction of immune-suppressants and donor lymphocyte infusion successfully related with long term survival. (data will be shown in ASH) Thus, the tight monitoring according to the mathematical model is important. The current strategy may be applied to other leukemia in which MRD monitoring by PCR is established.
Miyamura:Bristol-Myers Squibb Co., Ltd.:Honoraria;Celgene Co., Ltd.:Honoraria;Daiichi-Sankyo Co., Ltd.:Honoraria;Otsuka Co., Ltd.:Honoraria;Pfizer Co., Ltd.:Honoraria;Novartis Co., Ltd.:Honoraria.Goto:Takeda Pharmaceutical Co., Ltd:Honoraria;Novartis Pharma Co., Ltd.:Honoraria.Morishita:Bristol-Myers Squibb Co., Ltd.:Honoraria.Ozawa:Novartis Co., Ltd.:Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal